21st November 2019
John Collins, Chief Operating Officer of CIMIT, and Jorge‑Fernandez Garcia, EIT Health Director of Innovation discuss approaches that can lead to successful healthcare innovation.
John Collins, Chief Operating Officer at CIMIT in Boston, US, is a tested leader in technology-driven businesses with more than 25 years of hands-on, international experience in managing profit and loss centers and creating value by identifying business opportunities and accelerating the development and commercialisation of innovative products and services.

Jorge‑Fernandez Garcia, EIT Health Director of Innovation, has more than 20 years of experience in healthcare and life sciences, the last ten years fully dedicated to innovation, technology and entrepreneurship, at the intersection of business, government, and academia.

Innovation has the potential to change the face of Europe. It has the potential to improve the way we live, the way we plan for the future, and the way we thrive as a continent (both politically and economically). In order to innovate effectively, however, crucial building blocks must be in place.
EIT Health seeks to contribute towards a stronger health ecosystem in Europe by overcoming fragmentation, increasing efficiency and breaking down barriers to innovation in healthcare. What does this mean? It means that all parts of the innovation puzzle should work together effectively, across borders. In Europe, there are often barriers to this vision of cooperation: we don’t speak the same languages (literally and figuratively), each country has their own individual health systems, and we can often be quite locally-minded, so that innovation isn’t easily shared across the continent. We need to overcome this fragmentation if we want to address the challenges that exist, increase efficiency and break down barriers. While we seek to develop a unified, efficient system, we also must support individual innovators in navigating the current fragmentation.

EIT Health is not alone in its desire to strengthen the health ecosystem and support innovators. Across the Atlantic, a Boston-based innovation body, the Consortia for Improving Medicine with Innovation and Technology (CIMT), shares these goals.
Founded more than 20 years ago – by Massachusetts General Hospital, Brigham and Women’s Hospital, Charles Stark Draper Laboratory, and Massachusetts Institute of Technology – CIMIT is now a consortium of 13 of the greater Boston area’s premier clinical, research and academic institutions. It includes the Harvard Medical School and its teaching hospitals, along with a growing list of national and international affiliates. In addition to working with EIT Health, CIMIT is collaborating with institutions such as the National Institutes for Health (NIH) in the United States, the National Health Services (NHS) in England, CIMTI and Biocat in Spain, and the HealthTEC consortium in Singapore, to accelerate innovations into clinical practice.
Facilitating the Healthcare Innovation Process
Teams of healthcare innovators often have great technical and clinical expertise, but lack commercialisation/implementation expertise. As a result, teams that are new to the process often “don’t know what they don’t know” and make avoidable mistakes that stall, and even fatally wound, the most promising innovations.
 Some of the more common mistakes made by inexperienced innovation teams include:
Some of the more common mistakes made by inexperienced innovation teams include:
- Making something nobody wants! This happens far too often, especially with “tech push” innovations, which involve building something because you can. These ideas are not as likely to succeed as “clinical pull” innovations, which address an important unmet need. With health innovation, it is just as important to know the system/procedures as it is to know the technology – for a solution to really fly, it must seamlessly integrate into the way that healthcare is delivered, and have broad support from clinicians who will administer it.
- Addressing a small need that has little chance of delivering ROI: The cost of getting a medical device on the market is large, and commercially motivated investors must see a large enough market and potential return to be interested.
- Neglecting the economic buyer: Healthcare is unlike most industries in that users of healthcare products and services are rarely the people who write the cheque. Too often start-ups don’t know who makes the buying decisions and so they do not establish an economic value proposition to convince the real buyers.
- Choosing the wrong regulatory and market entry strategy: Solving a large unmet need with a novel technology is exciting, but the risks and investment needed can be huge, often too high in the eyes of investors. Successful entrepreneurs will select the right regulatory pathway for their solution, spend time considering the right trials that will demonstrate safety, efficacy and health economics, and listen carefully to feedback from regulators, with an agile approach to responding to such feedback.
- Not building protection for the business: Investors know that success will lead to competition. Teams with a patent feel they are protected, but far too often they leave open the door to many other ways to solve the same problem. Without a robust patent strategy, including a clean “Freedom to Operate” assessment, investors will walk away.
The Healthcare Innovation Cycle
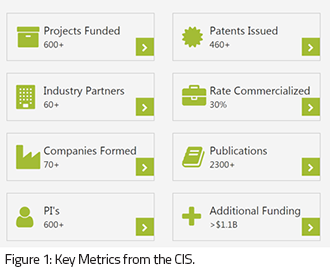
CIMIT took advantage of its more than 20 years of experience as a living lab of innovation in healthcare to conduct a retrospective review of its approach and to extract lessons learned. Through a clinical impact study (CIS), CIMIT evaluated the effectiveness of its approach in supporting innovators. The study found that innovative teams supported by CIMIT significantly exceeded industry norms in both the rate of successful commercialisation and the speed with which they reached the market. Some key findings are summarised in Figure 1.
CIMIT’s success in supporting innovation is based on engaging experienced entrepreneurs to facilitate teams in their journey. CIMIT facilitators (“Accelerator Executives”) have each started, managed, and exited healthcare start-ups. Their support has been crucial to success, as the reality is that most innovators only learn the process by trying – which is very inefficient in healthcare innovation given the timescales and expenses involved.
Beyond underlining CIMIT’s effectiveness, the study reached the simple but powerful conclusion that innovation in healthcare is a learnable, teachable process.
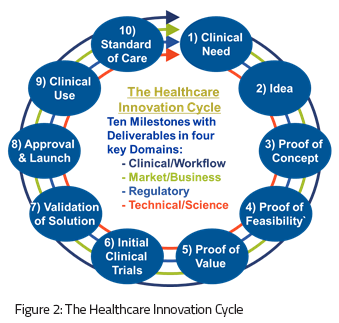
The process, called the Healthcare Innovation Cycle, is described as a sequence of healthcare-specific milestones with “deliverables” in four key domains critical to success in healthcare: clinical/workflow, regulatory, market/commercial, and technical/science (Figure 2). The process creates a roadmap that can guide teams as they navigate the complex journey from identifying an unmet clinical need to providing a solution that becomes the new standard of care, at which point the cycle starts again.
The way forward
Health innovators must ensure they are equipped with the relevant knowledge, support and access to networks of investors and partners, in order to develop real-world solutions that are market-ready. One error can prevent the most promising of innovations from improving patient care. Organisations like EIT Health and CIMIT are sharing best practices to provide services that support entrepreneurs and start-ups in healthcare, offering experienced guidance and training so that innovators do not need to go it alone.