18th April 2019
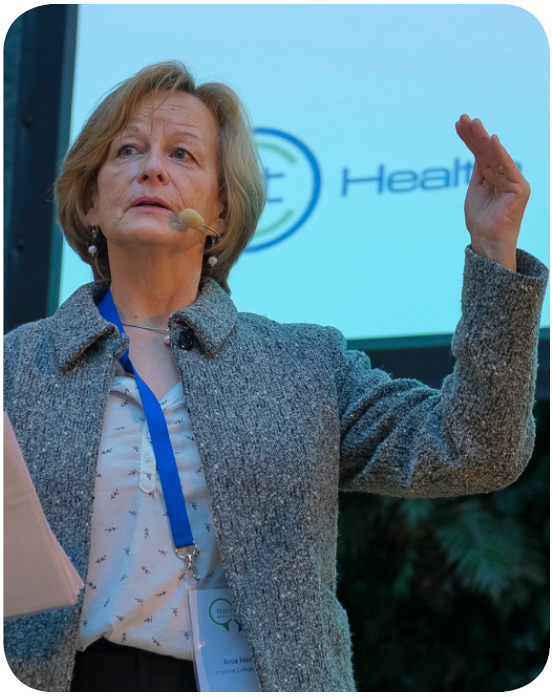
Ania Henley, Public Involvement Advisor at EIT Health Partner Imperial College, answers some of our questions on public involvement and public engagement in research.
Ania Henley is an adviser on the National Institute of Health Research (NIHR) Biomedical Research Centre (BRC) Patient and Public Panel at Imperial College, an EIT Health member. The panel’s remit is to influence PI at the strategic and governance level of research at Imperial. She also sits on the Medical Educational Ethics Committee (MEEC) at Imperial College and is the UK&IR representative on the Ethics Legal Social Issues (ELSI) board for EIT Health as the Lay Adviser. She also is a lay teacher on the EIT Health CRISH course.
Q: What are public involvement and public engagement?
A: Public Involvement (PI) is a form of citizen engagement that refers specifically to:
- Providing information and guidance to the public about research so that they can be more knowledgeable about the topic in general – known as “public engagement”.
- Getting members of the public involved in the organisation and governance of specific research projects – known as “public involvement”.
Q:What else do we mean when we talk about patient and citizen engagement?
A: Patient and citizen engagement within the health industry has grown exponentially in recent years – the well-known phrase, “nothing about us without us” encapsulates the ethical argument that public involvement is a right when a stakeholder group might be affected by a topic. It is essentially about ensuring that developments within the health sector – whether the development of a new medicine or technology, guidelines for the care of patients, or research – actively involve the people they are intended to serve. In terms of research, patients can help to facilitate the translation of research from “bench-to-bedside” by utilising their lived experience. Involving service users and the public in the research process may lead to research that better reflects the public’s needs and priorities. Ultimately, by making use of their knowledge, expertise and networks, researchers and innovators can provide more relevant solutions for the end user.

Q: Going back to PI specifically, how have you seen this area of patient engagement grow?
A: There are slight differences to the ways in which PI has developed in different countries across Europe, and definitions of what PI is are not uniform. Spain and France, for example, do not have a like-for-like concept of PI similar to the UK – where it is now mandatory in order for scientists to obtain public (and often private) funding for research. In the UK, PI goes beyond what we know as ‘public engagement’ and refers also to the process of patients and members of the public informing research from the point of view of their lived experience with the aim of enhancing it. Of course, involving patients in research and service provision does take place across the European Union, albeit using different terminology.

Q: What made you decide to get involved in research as a PI Adviser?
A: I spent 20 years working for Imperial College London creating systems which enabled the collection of data, for example research, audits and care pathways. I also co-ordinated clinical trials for the Orthopaedic and Cancer departments. It was while I was running these studies that I was asked if I would participate in a trial. My family suffered from various cancers and during this cancer trial, I would have regular scans and blood tests. This is what motivated me to get involved in research as a PI Advisor, and I am probably here to tell the story because I took part!
Q: Why should patients and the public get involved in research?
A:Research is paramount to ensure we save lives, and there are several arguments in favour of patient and public involvement in research. It makes a practical difference to the types of questions asked and the way that, for example, trials are run so it meets the needs of patients. It also improves the delivery and progression of research by looking at the feasibility and practicality of a study.What’s more, involving the public in research needn’t be complicated. You just need to remember that the point is to foster communication with people who have lived experience of specific health issues so that their insights can help inform translational research. Like so many people, I have been a patient (and will surely be again in the future). I have cared for members of my family and have learnt a lot in the process, and that experience can be extremely beneficial to research.
Q: How does EIT Health actively support the integration of patient and public engagement within its projects?
A: A great example of how PI is being supported by EIT Health is the CRISH Programme (Co-Creating Innovative Solutions for Health) led by the Barcelona Institute for Global Health. CRISH is a training course that teaches the public and professionals how to work together to co-create innovation for health. The co-creation approach being taught involves patients and their informal caregivers (family members) in the innovation process and allows them to learn how they can participate at key timepoints (for example, research) by sharing their experiences and ideas with other stakeholders, so that innovations better reflect the needs of patients and citizens. And that’s the key to public and patient involvement: seeing the public and patients as experts in their own right. Their expertise may be very different to those of researchers, but it is every inch as valuable!
PUBLISHED: 18 April 2019

